
Highlighted Paper: COVID-19 pneumonia: ARDS or not?
They say a picture is worth a thousand words. So that is what we wanted to start with! Do these two pictures look similar in your clinical judgement?
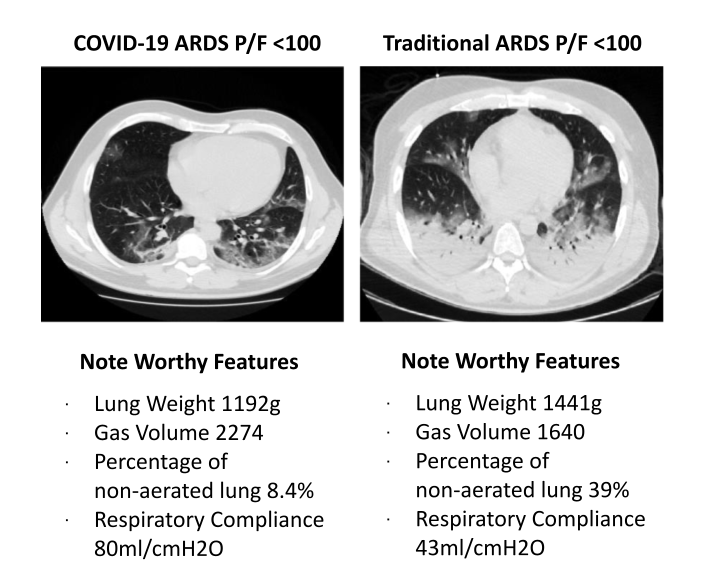
If your answer was no, then why would someone treat these two lungs the same in terms of ventilator management?
That is the very question we try to answer in this blog article. Some have called it COVID ARDS (CARDS), some Acute Vascular Disease (AVDS), but whatever we agree on calling it in the future, the commonality here is physicians and researchers trying to describe a new lung pathophysiology that they have not seen before the COVID-19 pandemic.
To try and make the differences between these two lung pathophysiologies as simple as possible, for the sake of clarity over the risk of oversimplification, let’s break the differences down to only two factors:
- Near normal versus a heavy lung weight – recall that in the traditional ARDS concept we see “capillary leak,” characterized by protein rich alveolar edema in the exudative phase, something not seen in COVID-19 ARDS
- Near normal versus decreased lung compliance – again, oversimplification is made here for the sake of clarity as in traditional ARDS in the later phases the lung will lose compliance, but in the earlier phases the “baby lung” concept may hold that the lung has nearly normal intrinsic elasticity¹
Let’s also break down traditional ARDSnet management strategy into two variables as well:
- Tidal Volumes – In traditional ARDS we target tidal volumes 4-8cc/kg, and ideally 4-6cc/kg if possible, as well as target Plateau Pressures of 30cmH20 or less, because in the “baby lung concept” we are concerned with ventilator induced lung injury (VILI) from stretch injury particularly in those alveolar segments that are open. Since the baby lung concept holds that only a small portion of the alveoli are actually available for gas exchange, maybe even as low as 20% of the lung, this small portion of the lung receives the full tidal volume given which places it at risk of overdistention, or stretch injury
- High PEEPs – PEEP is given based on the low or high peep arms of the ARDSnet protocol based on the rational that since in traditional ARDS the lung is laden with capillary leak and edema with high protein and atelectasis, high PEEPs are needed to “push” out this fluid and recruit alveoli
Before proceeding further, a special note is made here about driving pressures. Driving pressures are defined as P plateau-PEEP. You can see here that this difference in pressure will give you a tidal volume as you progressively increase PEEP for the patient to maximize their needed lung/alveolar recruitment. Instead of focusing on tidal volumes and plateau pressures separately this concept marries these two factors in a more dynamic physiological way. Ideally, we strive to maintain driving pressures <15cmH20. Perhaps then because of the real time relationship between tidal volumes and plateau pressures when driving pressures are monitored, several studies have found that this could be a superior strategy.²
I think with this clarity most, if not all of us, can start to see the problems of applying traditional ARDSnet strategies to the unique COVID-19 lung pathophysiology. They are:
- Traditional Tidal Volume Strategy – By applying lower tidal volumes to lungs that are compliant, this will be very uncomfortable to patients and likely require them to be sedated more for ventilator synchrony, or perhaps paralyzed. However, what we have learned from the recent literature on this topic is that this increased sedation requirement in COVID-19 ARDS is associated with an almost 6-fold increase in mortality³
- Traditional PEEP Strategy – What is the use of applying higher PEEPs to “recruit” a lung that is already open and aerated? None! In fact, this may lead to overdistension and worsening V/Q mismatch especially at higher respiratory rates >25/min, as well as possibly leading to barotrauma(4). Furthermore, alveolar OVERDISTENSION in an open/compliant lung may further lead to DEAD space ventilation. Particularly in COVID-19 this an important point to note because of the high incidence of coagulopathy seen in the disease which results in pulmonary micro thrombosis and right ventricular dysfunction as a result. This raises the interesting question if we should be monitoring ETCO2 in COVID-19 patients and calculate VD/VT via ETCO2/PaCO2?
Hopefully what is clear at this point is that we have been applying tools learned over two decades from the traditional ARDS lung model to the COVID-19 lung model that does not have the SAME or EVEN similar characteristics. As such it appears time for a change in the management paradigm.
In recognition of this and as a suggested management summary, Gattinoni has recommended the following ventilator management strategy in the COVID-19 ARDS patient:
- First and foremost is attention to the respiratory management of the patient prior to them becoming ICU status, or prior to their intubation. Here, the focus is on preventing further exacerbation of the VILI “vortex” to the point that they convert their COVID-19 ARDS pathophysiology from TYPE L (compliant lung) into a traditional ARDS lung (TYPE H) from their self-induced lung injury (SILI). The primary culprit here is the use of BiPap, and this is why HFNC is preferred. A review of this literature can be found here.
- PEEP levels should be limited to approximately 8-10 cmH2O, since higher levels will decrease pulmonary compliance and can impact right heart function.
- Tidal volumes should not be limited to 6 cc/kg. 8cc/kg appears safe in most patients, and if driving pressures are monitored perhaps these tidal volumes can be even slightly higher.
- Respiratory rate should not exceed 20 breaths/min.
- Patients should be left quiet with limited to no stimulation to avoid them increasing their respiratory drives and rate putting them at risk of SILI.
- Prone position is more likely to be a rescue maneuver only to facilitate the redistribution of pulmonary blood flow, rather than as a maneuver to open collapsed alveoli as in traditional ARDS. Hence, long term prone positioning is likely to be of little value.
- Monitoring of daily D-dimer levels and routine bedside echocardiography to assess for right heart function (see our highlighted paper on this topic here). This may provide guidance for therapeutic anticoagulation or the patients possible response to inotropes such as dobutamine, or vasodilators, such as nitric oxide or flonan.
- We suggest monitoring ETCO2 in COVID-19 patients by calculating VD/VT via ETCO2/PaCO2.
Authors:
Christopher Voscopoulos, MD, MBA, MS, MLS, FCCP, RPNI
President, Medical Specialists Associates
Board Certified in Anesthesiology, Critical Care, Neurocritical Critical Care, Pain Medicine, Addiction Medicine, Critical Care Echocardiography, Transesophageal Echocardiography, Obesity Medicine, and Board Eligible in Lifestyle Medicine. Registered Physician in Neuroimaging both Transcranial Doppler and Carotid Ultrasound
Nazir Habib, MD
Partner, Medical Specialists Associates
Board Certified in Internal Medicine and Critical Care
References:
- Gattinoni and Pesenti, “The Concept of ‘Baby Lung’.”
- Marini, “Evolving Concepts for Safer Ventilation.”
- Devlin and Pandharipande, “Do Our Sedation Practices Contribute to Increased Mortality in Coronavirus Disease 2019-Related Acute Respiratory Distress Syndrome?”; Wongtangman et al., “Association of Sedation, Coma, and In-Hospital Mortality in Mechanically Ventilated Patients With Coronavirus Disease 2019-Related Acute Respiratory Distress Syndrome: A Retrospective Cohort Study.”
- Gattinoni, Chiumello, and Rossi, “COVID-19 Pneumonia: ARDS or Not?”




